Super User
Bunions and Their Effects on Women

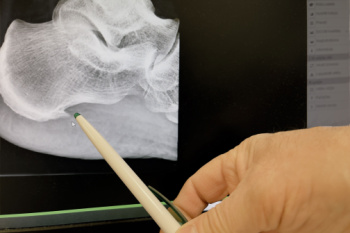
Bunions, or hallux valgus, disproportionately affect women, significantly impacting their overall foot health. Women are particularly susceptible due to factors like frequent wearing of high-heeled or narrow shoes, along with genetic predispositions. The risk of bunions has been shown to increase with age. The formation of a bunion starts with the big toe bending toward the smaller toes, which leads to a painful bony protrusion on the side of the foot. As bunions progress, they disrupt the alignment and function of adjacent toes. This often leads to formation of hammertoes or claw toes, altered weight distribution, corns and calluses. Research suggests that the severity of bunions correlates with increased pain not only in the feet but also in other parts of the body. Family history and flat feet are other contributing factors to the development of bunions. Addressing bunion deformity through early and effective interventions can offer significant relief and improve overall quality of life. If you are experiencing bunion-related discomfort, it is suggested that you make an appointment with a podiatrist for an exam and treatment.
If you are suffering from bunion pain, contact the foot specialists of Table Mountain Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Wheat Ridge, CO . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Symptoms and Management of Early Onset Gout

Early onset gout, a form of arthritis, can be a debilitating condition that disrupts daily life and impacts overall well-being. Gout typically manifests as sudden and intense pain, swelling, and tenderness in the joints, often affecting the big toe initially. This inflammatory response occurs due to the buildup of uric acid crystals in the joints, resulting from an imbalance in the body's production and excretion of uric acid. While gout is commonly associated with older age and certain lifestyle factors, like diet and alcohol consumption, it can also develop in younger individuals, often due to genetic predisposition or underlying health conditions. Managing early onset gout involves a multifaceted approach, including medication to alleviate symptoms, dietary modifications to reduce purine-rich foods, and lifestyle changes to maintain a healthy weight and minimize alcohol intake. Gout typically affects the big toe, and can cause severe pain and discomfort. If you have been afflicted with gout, it is suggested that you seek prompt attention from a podiatrist who can offer you relief and prevention methods.
Gout is a painful condition that can be treated. If you are seeking treatment, contact the foot specialists from Table Mountain Foot and Ankle. Our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our office located in Wheat Ridge, CO . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Definition and Causes of Clubfoot

Clubfoot, a congenital foot condition, manifests as a foot deformity characterized by inward rotation and bending of the ankle and foot. Understanding the definition, underlying causes, and frequency of occurrence of clubfoot is essential for early intervention and effective management. This condition occurs during fetal development when the tendons and ligaments in the foot are abnormally tight, causing the foot to twist inward. The exact cause of clubfoot remains unclear, although genetic factors and environmental influences are believed to play a role. While the majority of clubfoot cases occur sporadically without a family history, genetic predisposition can increase the likelihood of its occurrence. Clubfoot affects approximately one in every 1,000 newborns worldwide, making it one of the most common congenital musculoskeletal anomalies. Prompt diagnosis and treatment, typically through casting, stretching, and sometimes surgery, can help correct the deformity and improve the child's ability to walk and participate in activities as they grow. If your child has been born with clubfoot, it is strongly suggested that you are under the care of a podiatrist who can offer appropriate treatment solutions.
Congenital foot problems require immediate attention to avoid future complications. If you have any concerns, contact the foot specialists of Table Mountain Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
Congenital foot problems are deformities affecting the feet, toes, and/or ankles that children are born with. Some of these conditions have a genetic cause while others just happen. Some specific foot ailments that children may be born with include clubfeet, polydactyly/macrodactyly, and cleft foot. There are several other foot anomalies that can occur congenitally. What all of these conditions have in common is that a child may experience difficulty walking or performing everyday activities, as well as trouble finding footwear that fits their foot deformity. Some of these conditions are more serious than others. Consulting with a podiatrist as early as possible will help in properly diagnosing a child’s foot condition while getting the necessary treatment underway.
What are Causes of Congenital Foot Problem?
A congenital foot problem is one that happens to a child at birth. These conditions can be caused by a genetic predisposition, developmental or positional abnormalities during gestation, or with no known cause.
What are Symptoms of Congenital Foot Problems?
Symptoms vary by the congenital condition. Symptoms may consist of the following:
- Clubfoot, where tendons are shortened, bones are shaped differently, and the Achilles tendon is tight, causing the foot to point in and down. It is also possible for the soles of the feet to face each other.
- Polydactyly, which usually consists of a nubbin or small lump of tissue without a bone, a toe that is partially formed but has no joints, or an extra toe.
- Vertical talus, where the talus bone forms in the wrong position causing other bones in the foot to line up improperly, the front of the foot to point up, and the bottom of the foot to stiffen, with no arch, and to curve out.
- Tarsal coalition, when there is an abnormal connection of two or more bones in the foot leading to severe, rigid flatfoot.
- Cleft foot, where there are missing toes, a V-shaped cleft, and other anatomical differences.
- Macrodactyly, when the toes are abnormally large due to overgrowth of the underlying bone or soft tissue.
Treatment and Prevention
While there is nothing one can do to prevent congenital foot problems, raising awareness and receiving neonatal screenings are important. Early detection by taking your child to a podiatrist leads to the best outcome possible.
If you have any questions please feel free to contact our office located in Wheat Ridge, CO . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Congenital Foot Problems
A congenital foot problem is a problem affecting the feet, toes, and/or ankle that a child is born with. Several issues with a child’s feet can occur congenitally. Such problems include clubfoot, vertical talus, tarsal coalition, polydactyly, macrodactyly, and cleft foot. Some of these problems have a genetic basis, with someone in their family history having a gene causing the condition, and some are simply an anomaly.
The following are specifics about a few of these conditions:
- Clubfoot, also called congenital talipes equinovarus or talipes equinovarus, is When the tendons of the foot shorten, the bones are of an unusual shape, and the Achilles tendon is tight, causing an inward and downward pointing of the foot. The soles of the feet might also face each other. In most cases of clubfoot, both feet are affected. If not treated, the affected child will walk on the sides of their feet or ankles.
- Polydactyly is a condition where the child has more than five fingers or toes on either or both feet. Presentation usually consists of a nubbin or small lump of tissue without a bone, a toe that is partially formed but has no joints, or an extra toe.
- Vertical talus is where the talus bone forms in the wrong position, other bones in the foot do not line up properly, the front of the foot points up, and the bottom of the foot is stiff, has no arch, and usually curves out. This can occur in one or both feet and if left untreated, can lead to serious disability or discomfort as the child grows.
- Tarsal coalition is when there is an abnormal connection of two or more bones in the foot leading to severe, rigid flatfoot. The tarsal bones, located toward the back of the foot and in the heel, are the ones affected. This condition is often present at birth, but signs of the disorder usually come on in early adolescence.
- Cleft foot is a rare condition where the foot has missing toes, a V-shaped cleft, and other anatomical differences. Surgery can often help improve the foot’s function since the heel remains normal and is what is most needed for walking. The main issues with this affliction are whether the affected foot can fit into a shoe and the shape and appearance of the foot.
- Macrodactyly is when the toes are abnormally large due to overgrowth of the underlying bone or soft tissue. Having this condition makes it harder for the child to use the affected foot for certain activities.
Essential Foot Care Tips for Seniors

As you age, your feet require extra attention and care to maintain mobility and overall well-being. Proper foot care is essential for seniors to prevent common issues such as foot pain, infections, and injuries. Regular inspection of the feet is vital, and this includes checking for cuts, sores, or signs of infection, especially for those with diabetes or circulatory issues. Keeping the feet clean and dry, including thorough drying between the toes, helps prevent fungal infections like athlete's foot. Seniors should wear comfortable, properly fitting shoes with adequate support and cushioning to reduce pressure and friction on the feet. Regular foot exercises and stretches can improve circulation, flexibility, and strength, enhancing balance and reducing the risk of falls. Additionally, maintaining a healthy lifestyle with proper nutrition and hydration supports overall foot health. If you are a senior experiencing foot pain, it is strongly suggested that routine appointments are scheduled with a podiatrist who can provide you with relief options.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact the foot specialists from Table Mountain Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our office located in Wheat Ridge, CO . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Advantages and Drawbacks of Laser Treatment for Toenail Fungus

Laser treatment for fungal nails has drawn attention as a potential solution for addressing this common and often stubborn condition. One of the significant advantages of laser therapy is its non-invasive nature, offering a relatively painless and quick procedure compared to traditional treatments like oral medications or topical antifungal creams. Laser treatment targets the fungus directly, penetrating the nail bed without causing damage to surrounding tissues. Additionally, it typically requires minimal downtime, allowing patients to resume their daily activities immediately after the procedure. However, laser therapy may not be suitable for everyone, and its efficacy varies among individuals. Some individuals may require multiple sessions to achieve satisfactory results, and there is no guarantee of complete eradication of the fungal infection. Overall, while laser therapy presents potential benefits for treating fungal nails, patients should weigh these against the associated drawbacks and consider all treatment options in consultation with their podiatrist. If you have toenail fungus and are considering this type of treatment, it is suggested that you speak with this type of doctor who can address any concerns you may have.
Laser treatment can be an effective way to get rid of toenail fungus. If you have any questions about laser treatment, consult with the foot specialists from Table Mountain Foot and Ankle. Our doctors will assess your condition and provide you with quality treatment for fungal nails.
What Are Toenail Fungal Infections?
Onychomycosis, or fungal infection of the nail, is a relatively common and non-serious condition. Around 10 percent of U.S. citizens are afflicted with fungal nails. Common forms of fungus that infect the nail include dermatophytes, yeasts, and molds.
Symptoms of Toenail Fungal Infections Include:
- Nail thickening
- Brittleness of the nail
- Discoloration of the nail
Diagnosis for Fungal Nails
Fungal infections are diagnosed by fungal culture and microscopy. This will rule out any other conditions such as nail trauma, psoriasis, lichen planus, and onychogryphosis.
What Is Laser Treatment?
Laser treatment is a non-invasive, safe, quick, and painless procedure that uses the heat from a laser to kill fungus in the nail. Each infected nail is targeted with a laser for several minutes. The treatment is usually utilized several different times over a select period. During this time, a podiatrist will keep an eye on the infection.
If you have any questions, please feel free to contact our office located in Wheat Ridge, CO . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Laser Treatment for Fungal Nails
A new treatment for fungal nails, or onychomycosis, which has grown in popularity in recent years, is laser treatment. Laser treatment involves the use of a laser that kills fungus in the toenail with heat. Laser therapy causes no side effects and does not affect nearby healthy tissue.
Toenail fungus afflicts almost 10 percent of the U.S. population and is more common among the elderly. The most common symptom of toenail fungus is the discoloration and thickening of the nail. The nail can also become brittle and a foul smell may be produced. In rare cases, pain might be present. While it is not a serious condition, it can lead to a perception of disgust amongst those it affects. There are several different fungi that cause fungal infections. These include dermatophyte, yeast, and mold. The most common of these is dermatophyte.
Diagnosis for fungal nails involves a podiatrist utilizing microscopy and fungal cultures. This will allow the doctor to determine whether it is a fungus or another condition, such as lichen planus, psoriasis, nail damage, and onychogryphosis.
Fungus in the nails can be hard to get rid of with over-the-counter drugs. This is due to the nail being hard and protective, with fungus able to slip between the nail bed and plate. Furthermore the slow growth of the nail increases the difficulty of fungus going away. Laser treatment seeks to get around this by directly penetrating through the nail and killing the fungus. The laser is used on each infected nail for a couple of minutes. Patients then typically return several weeks or months later for another laser treatment. During this time the podiatrist will routinely observe the foot and infection. It is also recommended to wear clean socks and shoes and allow the feet to dry and breathe to prevent toenail fungus.
Laser treatment is still a relatively new treatment and not all podiatrists have laser machines. Ask your podiatrist if they do laser treatment for toenail fungus and if it is right for you.
Common Causes of Swollen Feet

Swollen feet, an uncomfortable condition, can stem from various factors, necessitating attention and understanding to alleviate symptoms effectively. One common cause is prolonged standing or sitting, which can impair circulation and lead to fluid retention in the feet and ankles. Additionally, injuries such as sprains or fractures may result in localized swelling as the body responds to tissue damage. Certain medical conditions, including venous insufficiency and lymphedema, disrupt the normal flow of fluids in the body, contributing to swelling in the lower extremities. Lifestyle factors like excessive salt intake, obesity, and dehydration can exacerbate fluid retention and swelling in the feet. Pregnancy often leads to swollen feet due to hormonal changes and increased pressure on the blood vessels. If your feet have become swollen, it is suggested that you schedule an appointment with a podiatrist who can determine what the cause is, and offer appropriate treatment solutions.
Swollen feet can be a sign of an underlying condition. If you have any concerns, contact the foot specialists of Table Mountain Foot and Ankle. Our doctors can provide the care you need to keep you pain-free and on your feet.
Swollen feet are a common ailment among pregnant women and people who stand or sit for extended periods. Aging may increase the possibility of swollen feet and patients who are obese often notice when their feet are swelling too. There may be medical reasons why swollen feet occur:
- Phlebitis - A condition that causes the veins to become inflamed and can also cause leg pain.
- Liver disease - This may lead to low blood levels of albumin which is a protein. This can cause fluid in the blood to pass into the tissues and several areas of the body can become swollen.
- Heart failure - When the heart doesn’t pump properly the blood that is normally pumped back to the heart can pool in the veins of the legs causing swollen feet.
- Kidney disease - One of the main functions of the kidneys is releasing excess fluid in the body. This type of condition can make it difficult for the kidneys to function properly, and as a result the feet may become swollen.
- Deep-vein thrombosis (DVT)- This is a serious condition where blood clots form in the veins of the legs. They can block the return of blood from the legs to the heart which may cause the feet to swell. It is important to be treated by a podiatrist if this condition is present.
Swollen feet can also be caused by bone and tendon conditions, including fractures, arthritis, and tendinitis. Additionally, there may be skin and toenail conditions and an infection may cause the feet to swell. Patients who take medicine to treat high blood pressure may be prone to getting swollen feet.
Many patients elevate their feet to help relieve the swelling and this is generally a temporary remedy. When a podiatrist is consulted the reason behind the swelling can be uncovered and subsequently treated.
If you have any questions please feel free to contact our office located in Wheat Ridge, CO . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Understanding the Potentially Debilitating Effects of Heel Spurs
Heel spurs, bony protrusions that develop on the underside of the heel bone, can pose significant challenges for individuals affected by this condition. While not always painful, heel spurs have the potential to become debilitating, causing discomfort and limiting mobility. These spurs often result from repetitive strain or stress on the foot, commonly associated with conditions like plantar fasciitis or excessive pronation. As the body attempts to repair itself, calcium deposits accumulate, leading to the formation of a spur. The presence of a heel spur can exacerbate existing foot conditions, causing sharp pain and tenderness, especially during weight-bearing activities such as walking or running. Left untreated, heel spurs may interfere with daily activities and quality of life, impacting overall well-being. Early diagnosis and intervention are vital for managing symptoms and preventing further complications associated with heel spurs. Seeking professional guidance from a podiatrist can help individuals effectively address heel spurs and regain optimal foot health. If you have a heel spur, it is suggested that you are under the care of this type of doctor who can help you manage this condition.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact the foot specialists from Table Mountain Foot and Ankle. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Wheat Ridge, CO . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.







